Heart and circulatory diseases don’t usually appear out of nowhere. They build quietly over the years, shaped by a combination of genetics, lifestyle, environment, and sometimes even habits we don’t realize are affecting our health. At Advanced Cardiovascular Specialists, we see every day how early awareness can change the trajectory of a patient’s life. When people understand their risk factors, they’re able to make smarter decisions, catch issues earlier, and stay ahead of serious disease.
This guide breaks down the major risk factors for heart and circulatory diseases, explains why they matter, and shows you how even small changes can support long-term cardiovascular health.
Understanding Cardiovascular Risk
Risk factors fall into two big categories: those you can control and those you can’t. Things like age and genetics are outside of your control, but your lifestyle, daily habits, and medical conditions are not. Most patients have a mix of both, and the key is learning how they interact.
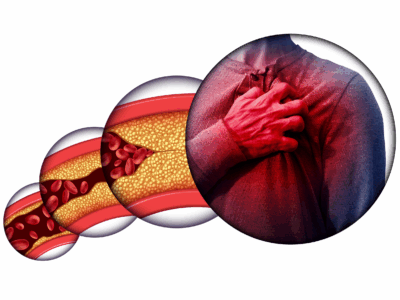
Cardiovascular disease develops when the heart or blood vessels become damaged, weakened, or obstructed. High blood pressure, plaque buildup, blood sugar irregularities, and inflammation can all play a role. Over time, these problems increase the likelihood of heart attack, stroke, heart failure, arrhythmias, and circulation issues like peripheral artery disease.
The goal isn’t perfection. It’s progress. The more you understand your risks, the more power you have to protect your heart.
Major Risk Factors You Can Control
These are the risk factors that respond most directly to lifestyle changes and medical treatment. Addressing them often creates a ripple effect that improves your overall cardiovascular health.
1. High Blood Pressure
High blood pressure (hypertension) is one of the strongest predictors of heart disease. When blood pressure stays elevated, your heart has to work harder to pump blood, which strains the heart muscle and damages artery walls.
Because hypertension often has no symptoms, many people don’t know they have it. Regular screenings are essential. If your blood pressure is consistently high, lifestyle changes and medication can help reduce your risk dramatically.
2. High Cholesterol
Cholesterol itself isn’t the villain. Your body needs it. But too much LDL cholesterol can contribute to plaque buildup inside the arteries, while too little HDL makes it harder for your body to clear that plaque.
This imbalance increases the risk of blockages that may lead to heart attack or stroke. Diet, exercise, and medications like statins play a major role in maintaining healthy levels.
3. Smoking and Tobacco Use
Smoking damages the lining of your blood vessels, increases plaque buildup, raises heart rate, and reduces oxygen in the blood. Even occasional or social smoking can elevate cardiovascular risk.
Quitting is one of the best decisions you can make for your heart. Within a year of stopping, your risk of heart disease drops significantly. If you need support, talk to your provider about cessation methods that work.
4. Diabetes
High blood sugar damages blood vessels and increases inflammation, which accelerates atherosclerosis. People with diabetes face a much higher risk of developing heart disease, often earlier in life.
According to the Centers for Disease Control and Prevention, people with diabetes are twice as likely to experience heart disease or stroke as those without it.
Managing blood sugar through diet, activity, medication, and routine monitoring is essential. Our team at Advanced Cardiovascular Specialists can help evaluate your risk and create a plan that protects both your heart and circulation.
5. Obesity
Excess weight contributes to several other risk factors like hypertension, high cholesterol, and diabetes. It also increases inflammation in the body and places added stress on the heart.
Even moderate weight loss, such as five to ten percent of your current weight, can create measurable improvements in cardiovascular health. Small, sustainable changes tend to work better over time than drastic short-term diets.
6. Sedentary Lifestyle
Your heart is a muscle. It needs regular activity to stay strong. A lack of movement slows circulation, contributes to weight gain, and increases the likelihood of blood pressure and cholesterol issues.
The American Heart Association recommends at least 150 minutes of moderate-intensity exercise per week. That doesn’t mean you need to run marathons. Walking, cycling, household chores, dancing, or gardening all count.
7. Poor Diet
A diet high in processed foods, saturated fats, sugar, and sodium makes it harder for your heart to function well. It contributes directly to plaque buildup, inflammatory responses, and weight gain.
Choosing whole foods, fiber, lean proteins, and heart-healthy fats can significantly reduce risk. Our providers can help you understand how nutrition shapes cardiovascular health and what dietary habits offer the most benefit.
Major Risk Factors You Cannot Control
Even though you can’t change these risk factors, understanding them helps you make more informed decisions about your lifestyle and screenings.
1. Age
The risk of heart and circulatory diseases increases as you get older. Arteries naturally stiffen with age, and the heart muscle may weaken over time.
This doesn’t mean cardiovascular disease is inevitable. It simply means that screenings become even more important once you reach your 40s, 50s, and beyond.
2. Family History and Genetics
Genetic predisposition plays a strong role in several types of heart disease, including coronary artery disease, arrhythmias, cardiomyopathy, and high cholesterol. If a biological parent or sibling developed heart disease before age 55 for men or 65 for women, your risk is higher.
If heart problems run in your family, a preventive evaluation at Advanced Cardiovascular Specialists is a smart step forward. Early detection changes outcomes.
3. Sex and Hormonal Factors
Men typically face higher cardiovascular risk earlier in life, while women see their risk climb sharply after menopause. Hormonal changes impact cholesterol levels, blood pressure, and inflammation in ways that play a role in heart health.
Women may also experience different symptoms during heart events, making awareness even more important.
4. Ethnicity
Certain populations face higher risk due to genetic and environmental factors. For example, African American adults are more likely to develop high blood pressure and experience complications from it. Hispanic and Native American populations also show higher rates of diabetes, which raises cardiovascular risk.
This is why personalized care and culturally aware prevention strategies matter when assessing long-term heart health.
Conditions That Increase Cardiovascular Risk
Heart disease and circulatory disease often overlap, but circulatory conditions specifically affect blood flow throughout the body. These include peripheral artery disease (PAD), blood clots, venous insufficiency, and aneurysms.
Here are the major contributors:
1. Atherosclerosis
This is the root cause behind most circulatory problems. When plaque builds up inside arteries, it narrows the pathways your blood relies on. This can lead to leg pain while walking, cold limbs, poor wound healing, or even dangerous blockages.
2. High Blood Pressure
Hypertension damages blood vessels over time, making them less elastic. This increases the risk of aneurysms, strokes, and circulation issues in the legs.
3. Obesity and Inactivity
When blood flow slows due to inactivity or excess weight, veins and arteries struggle to move blood efficiently. This creates an environment where clots and blockages are more likely to form.
4. Smoking
Smoking decreases circulation, hardens arteries, and lowers oxygen levels in the bloodstream. Even short-term exposure can impact vascular health.
5. Diabetes
Blood sugar fluctuations damage blood vessels and nerves, which slows circulation. Diabetes is one of the strongest predictors of peripheral artery disease.
Warning Signs of Cardiovascular Risk
Even if you feel healthy, your body may be giving you clues that your risk is increasing.
Be aware of the following symptoms:
- Chest pain or tightness
- Shortness of breath
- Irregular heartbeat
- Leg pain during walking
- Numbness or coldness in the limbs
- Swelling in the legs or ankles
- Sudden fatigue or dizziness
If you notice symptoms like these, schedule an evaluation. Early testing can identify problems before they become emergencies.
How Advanced Cardiovascular Specialists Can Help
When it comes to preventing heart and circulatory diseases, knowledge and early intervention make all the difference. At Advanced Cardiovascular Specialists, we provide comprehensive evaluations, diagnostic testing, and personalized treatment plans that support long-term cardiovascular health.
Whether you’re managing high blood pressure, monitoring cholesterol, concerned about family history, or experiencing symptoms for the first time, our team is here to help you take control of your heart health.
Take Charge of Your Heart Health Today
Cardiovascular risk isn’t something to fear. It’s something to understand. Every risk factor you identify gives you a new opportunity to make meaningful change. With a combination of medical guidance and simple lifestyle adjustments, you can protect your heart and circulation for the long term.
If you’re ready for a personalized evaluation or want to better understand your risks, reach out to Advanced Cardiovascular Specialists. Your heart works hard for you every day. Take the next step to protect it.

 The Role of Gut Health in Cardiovascular Wellness
The Role of Gut Health in Cardiovascular Wellness